01 Cardiac Anatomy
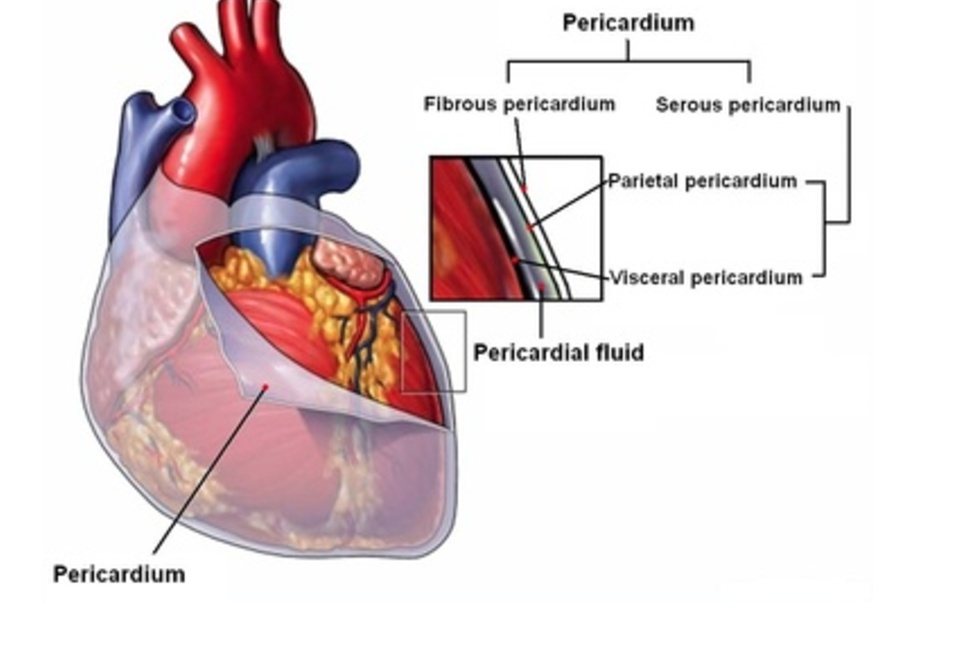
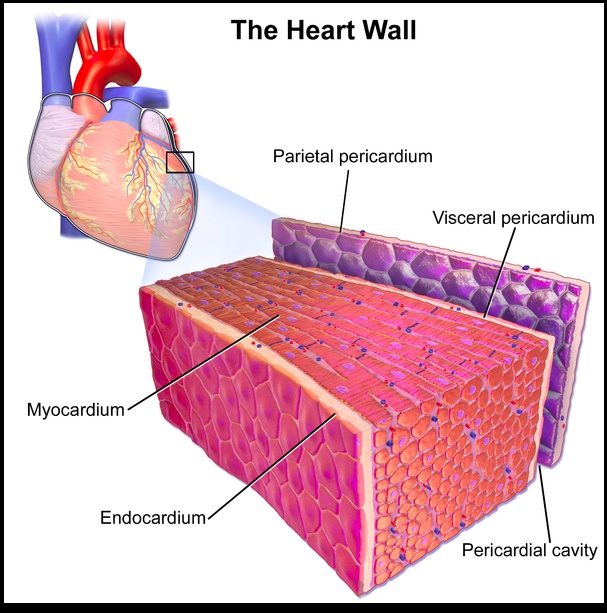
Pericardium
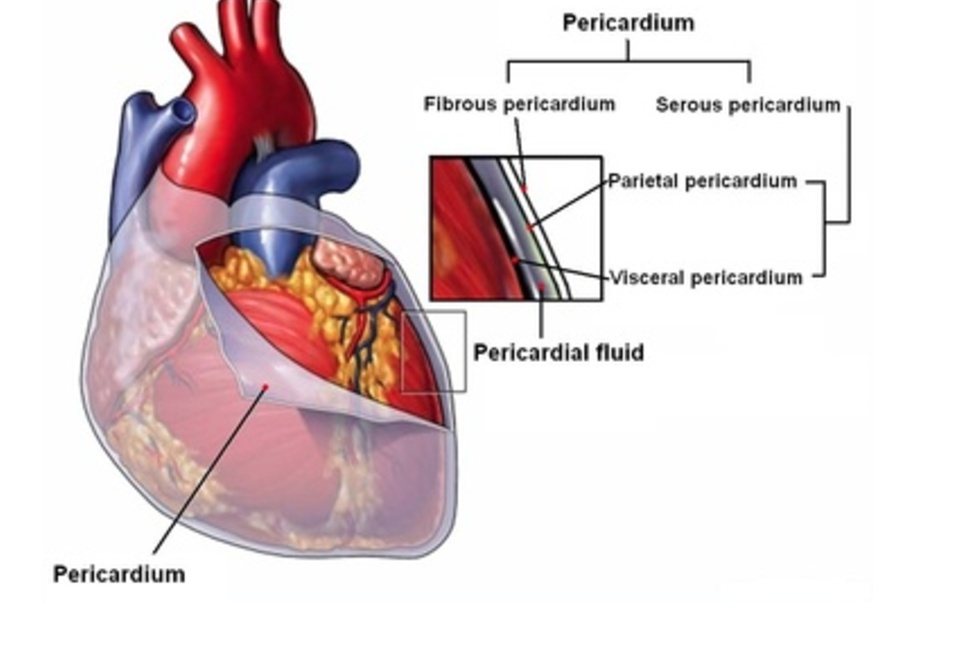
The pericardium is double-walled sac that encloses the heart and great vessel roots.
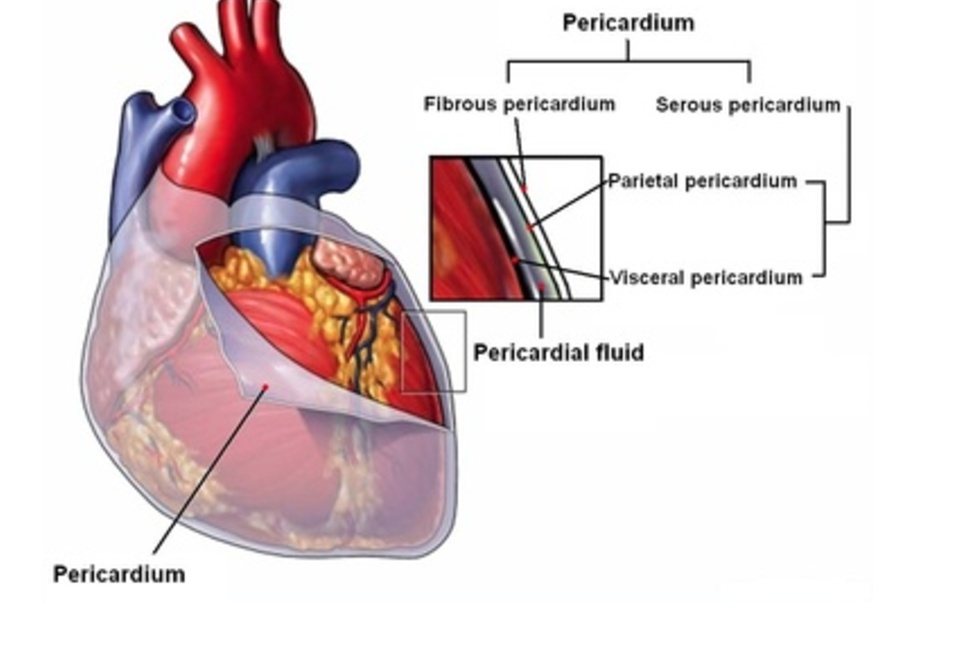
Pericardium composed of 2 layers:
- Fibrous pericardium on outside
- Serous pericardium on inside, made up of parietal and visceral layers.
Fibrous Pericardium
Strong external layer that limits the expansion of the pericardial cavity; it is continuous with the adventitia that surrounds the great vessels entering and exiting the heart.
Fused to the diaphragm on its inferior surface and is anchored to the sternum by connective tissue called the sternopericardial ligaments.
Serous Pericardium
Composed of parietal and visceral layers:
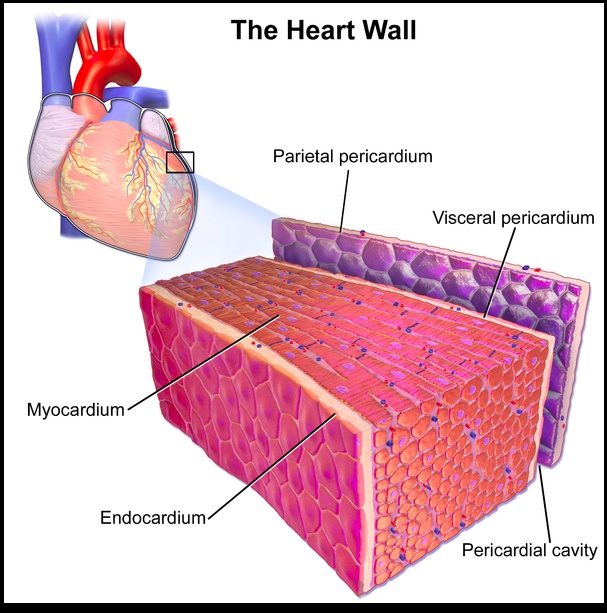
- Parietal layer: The parietal layer forms the inner layer of the fibrous pericardium and is the most external layer of the serous pericardum; it is fused to the fibrous pericardium, which is external to the parietal layer.
- Visceral layer (epicardium): The visceral layer covers the external surface of the heart itself and is the innermost layer of the pericardium deep to the parietal layer and fibrous pericardium.
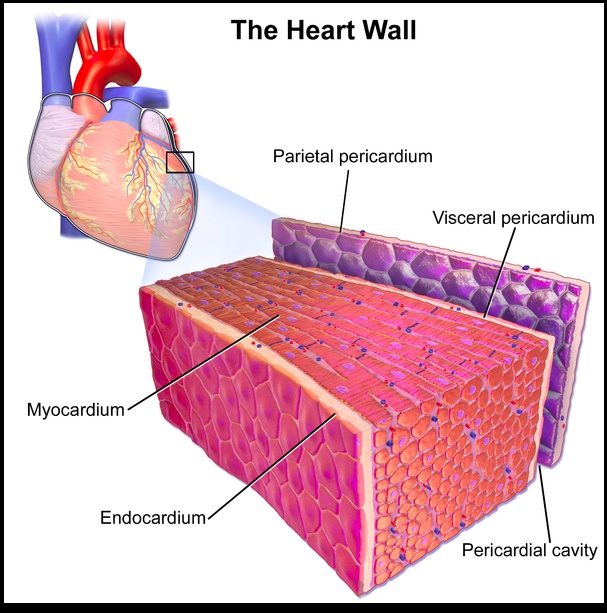
Pericardial fluid collect between visceral and parietal layer of serous pericardium, the pericardial cavity.
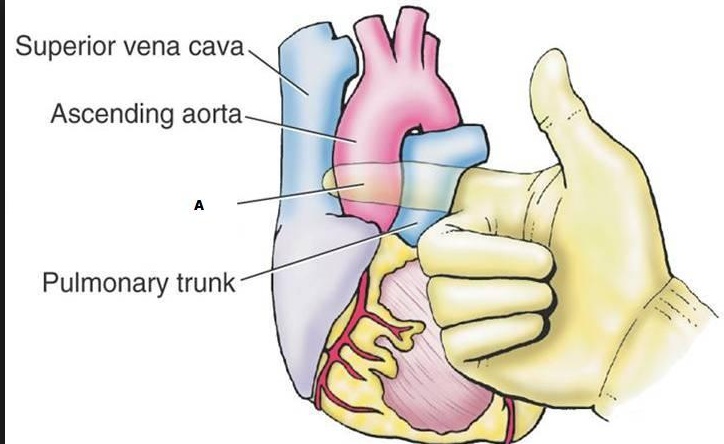
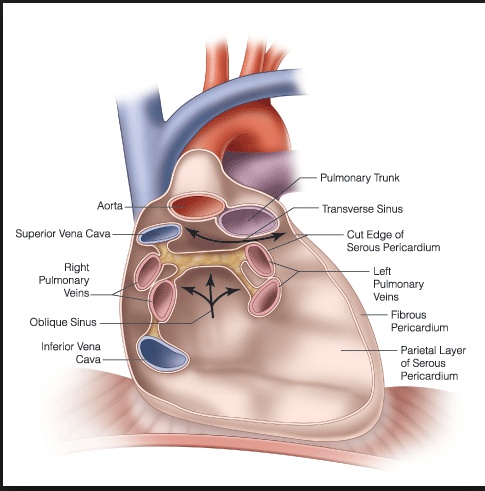
Transverse pericardial sinus
An anatomical space within the pericardial cavity posterior to the pulmonary trunk and ascending aorta but anterior to the superior vena cava.
Oblique pericardial sinus
Space on the posterior aspect of the left atrium; it is formed by reflections of pericardium from where the IVC, SVC, and pulmonary veins enter into the heart. The right border is formed by the IVC and right pulmonary veins and the left border is formed by the left pulmonary veins.
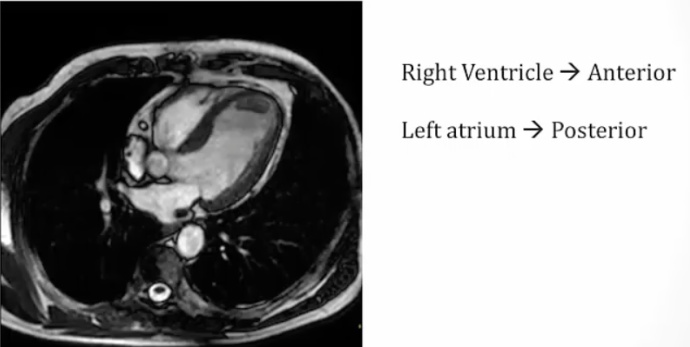
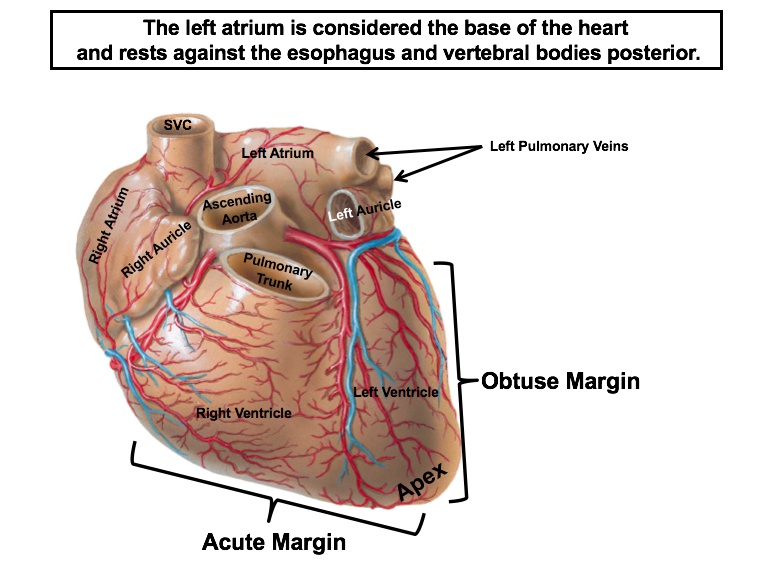
Posterior heart surface
Defined by left atrium and a portion of the right atrium.
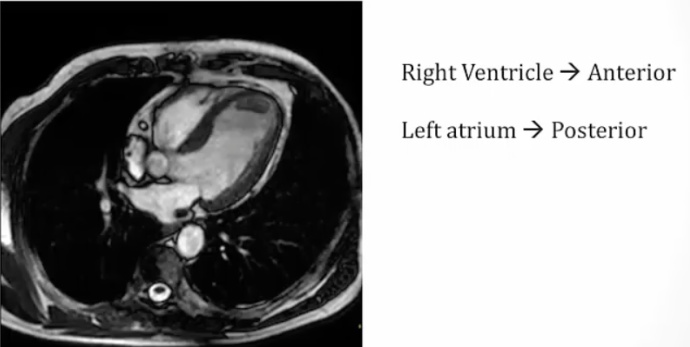
Esophagus sits between LA and aorta.
Diaphragmatic surface
Aka inferior surface of heart.
Comprised by 2/3 of the left ventricle and 1/3 of the right ventricle.
Coronary Sulcus
Separates the ventricles and atria are circumferentially.
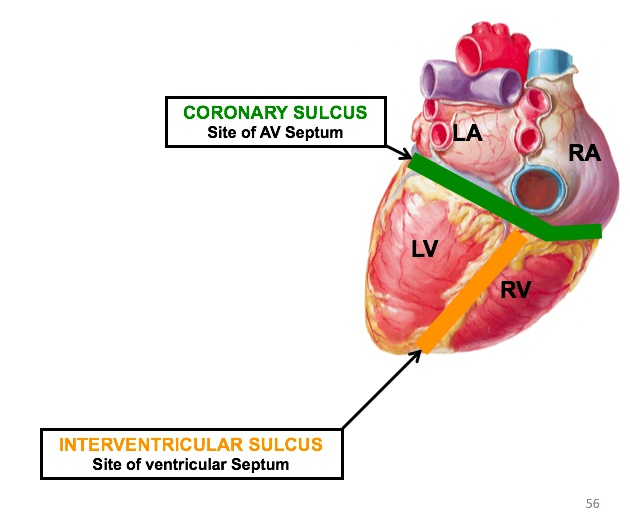
The structure is also known as the coronary or atrioventricular groove.
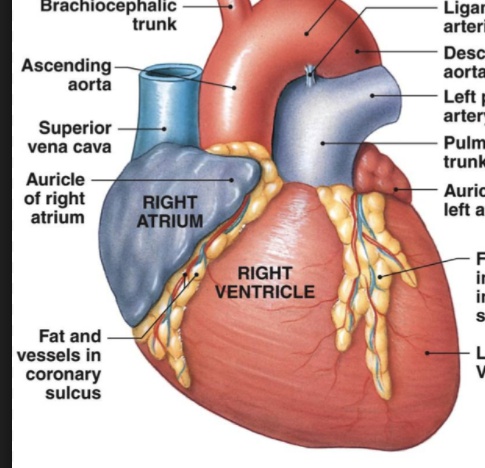
Sternocostal surface
Aka anterior surface of heart.
Is comprised of 2/3 right heart and 1/3 left heart — centrally by the RV and by the RA and LV on their corresponding sides.
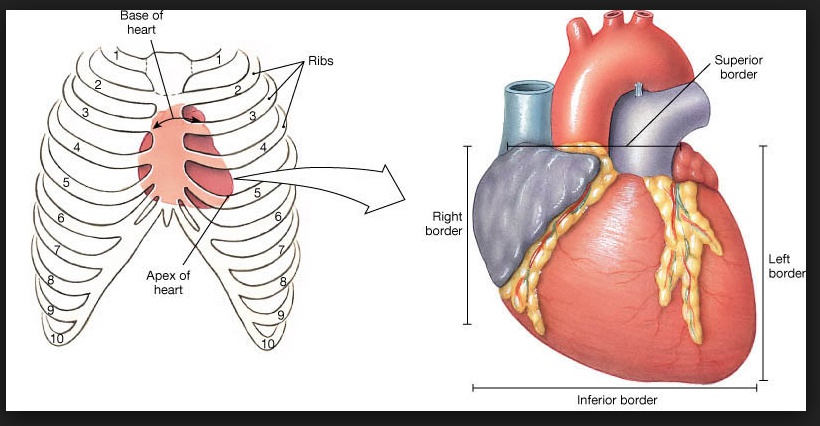
Heart Apex
Approximately 8 cm left of the median plane in the 5th intercostal space; formed by the left ventricle.
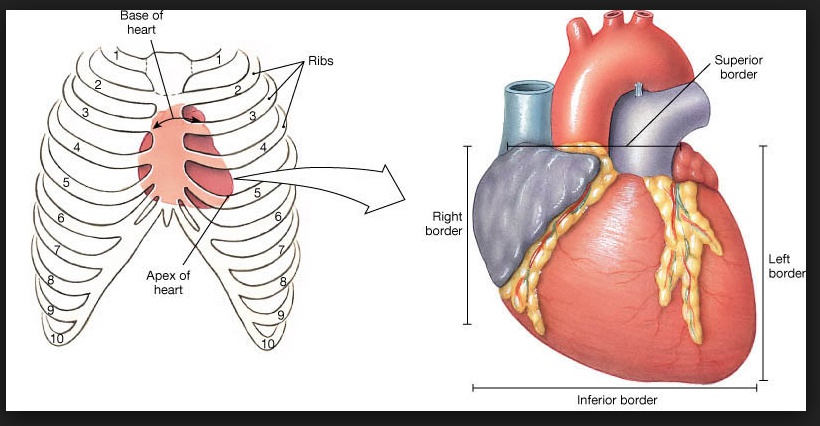
Heart Base
A region where the aorta, pulmonary trunk, and SVC emerge from the heart. Found immediately deep to the sternal angle and the left and right portions of the 2nd intercostal spaces. Left atrium is considered the base of the heart.
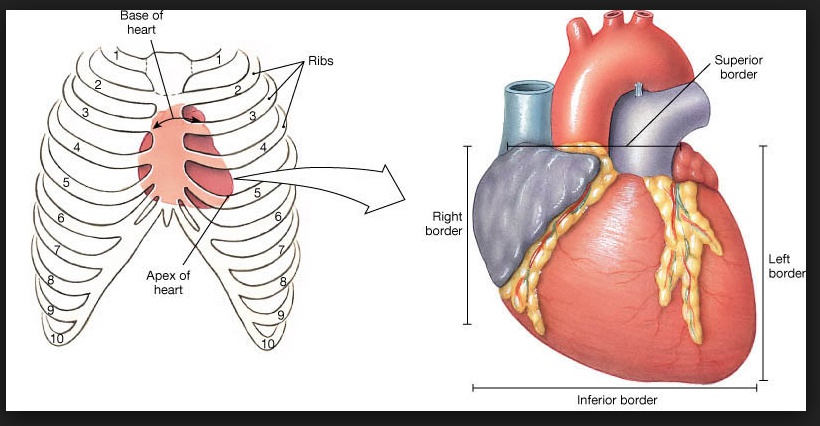
Heart Right Border
Formed by the right atrium.
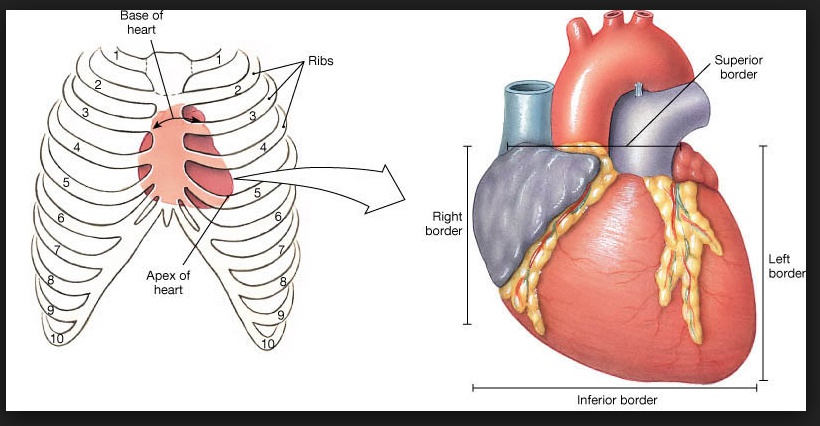
Heart Left Border
Formed by the left ventricle.
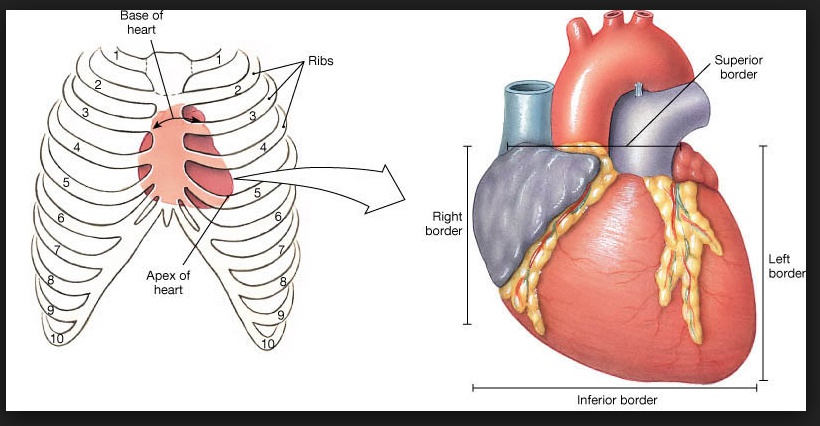
Heart Inferior Border
Formed by the right ventricle and a small portion of the left ventricle near the apex of the heart.
Internal Anatomy
Cardiac Myocytes form the myocardium on a microscopic level. They are precisely coordinated by gap junctions within intercalated discs that allow rapid spread of electrical signals between cells.
SA Node
The pacemaker of the heart. Exhibits automaticity by spontaneously generating action potentials. Located at the junction of the superior vena cava and the right atrium. Initiates the electrical impulses to stimulate contraction.
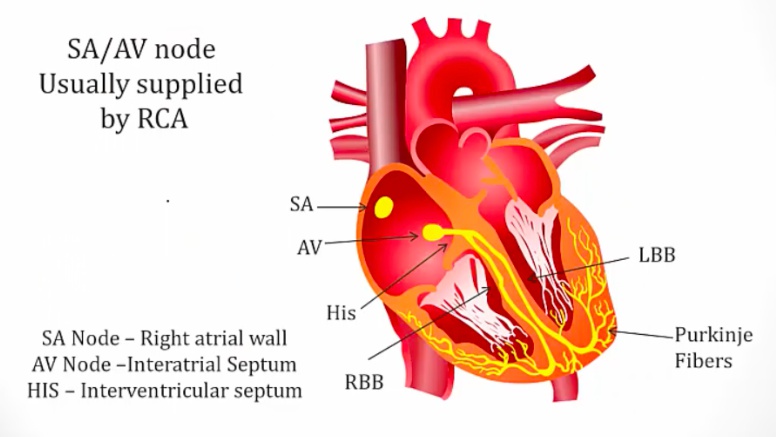
AV node
Located between the atria and ventricles and conducts the signal from the sinoatrial node to the rest of the heart. It slows down conduction between the atrium and the ventricles, allowing time for the ventricles to fill with blood before contraction.
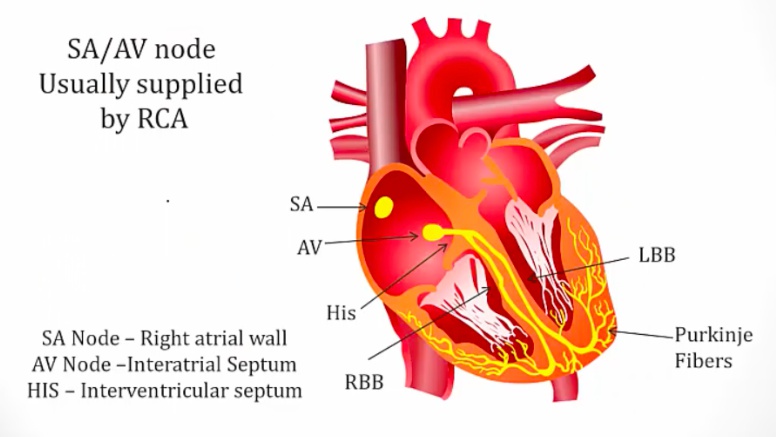
Bundle of His
Bundle of specialized cardiomyocytes (bigger cells with fewer contractile elements → less electrical resistance) that propagate signals from the AV node down into the ventricles. Clinical Correlate: Defects in the His-Purkinje system are responsible for second degree heart block: Mobitz type 2.
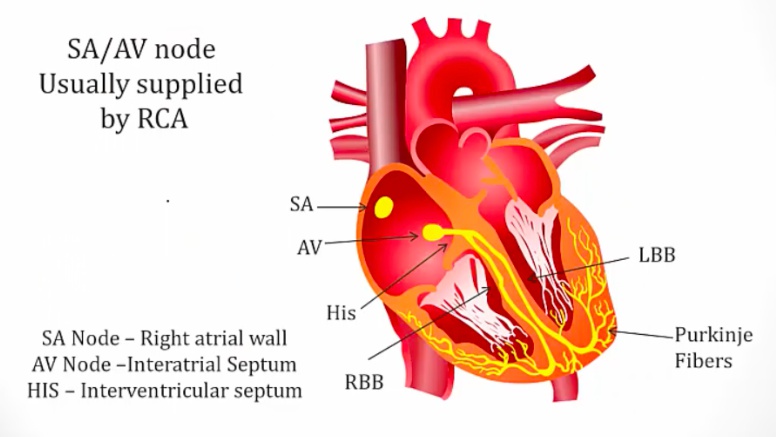
Left and Right Bundle Branches
Branches of the bundle of His that conduct to the left and right ventricles via Purkinje fibers. Clinical Correlate: These can become blocked in heart failure → left or right bundle branch block.
Purkinje fibers
Located along the edges of each ventricle, conduct the signal from the bundle of His and bundle branches to ventricular cardiomyocytes.
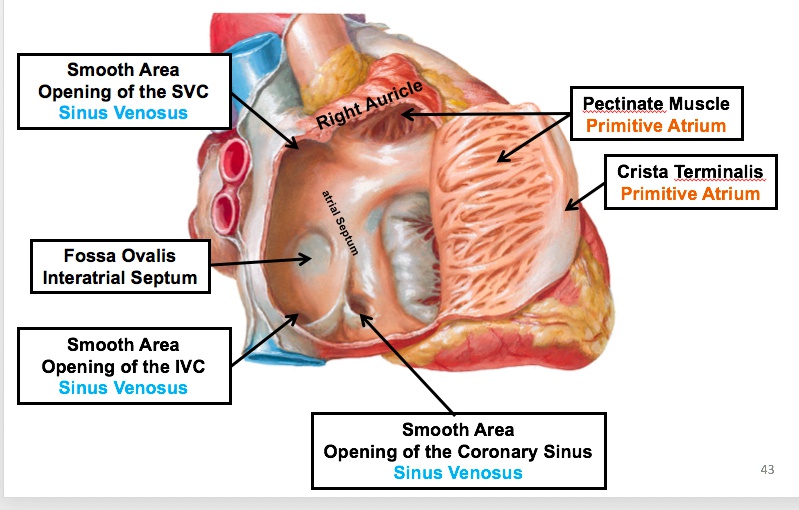
Right Atrium
Receives deoxygenated blood from the inferior vena cava, superior vena cava, and coronary veins.
Sinus Venarum
Smooth internal portion of the posterior right atrium in between the two vena cavae and includes the interatrial septum. It is the incorporated adult remnant of the embryonic sinus venosus. 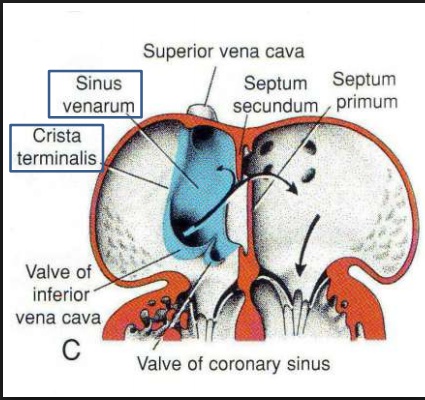
Crista Terminalis
Internal muscular ridge that divides the right atrium into the atrium proper and the vena caval area.
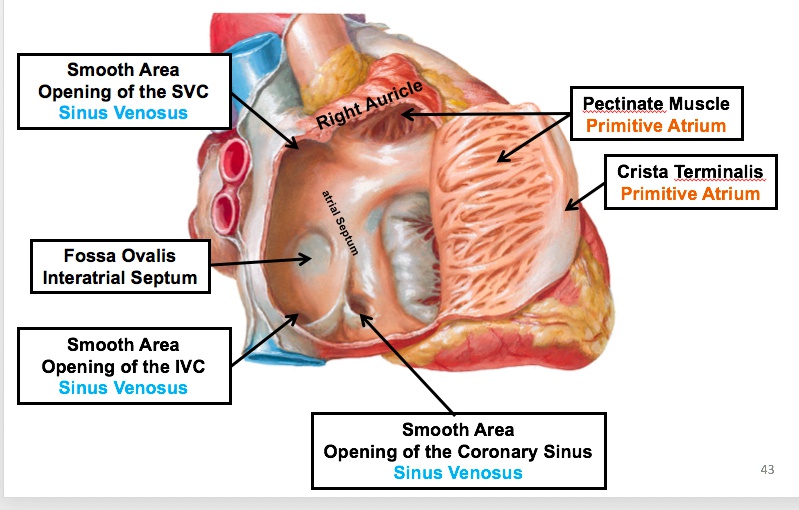
Atrium Proper
Trabeculated part of the right atrium lined with pectinate muscles, which are bundle muscle fibers found predominately within the auricle, an ear-shaped appendage. Note: Pectinate muscles are also present in the left atrium but are less prominent.
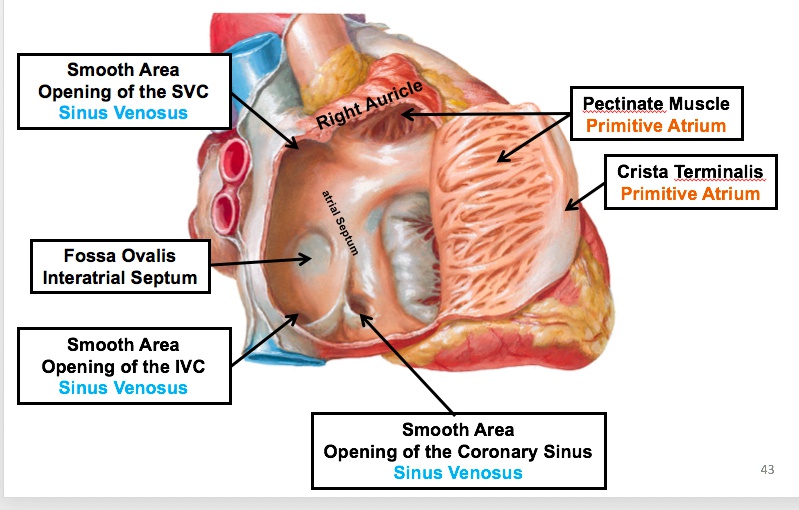
Fossa Ovalis
Depression in the interatrial septum and the remnant of the foramen ovale; lateral and superior borders form the limbus of the fossa ovalis.
Right Ventricle
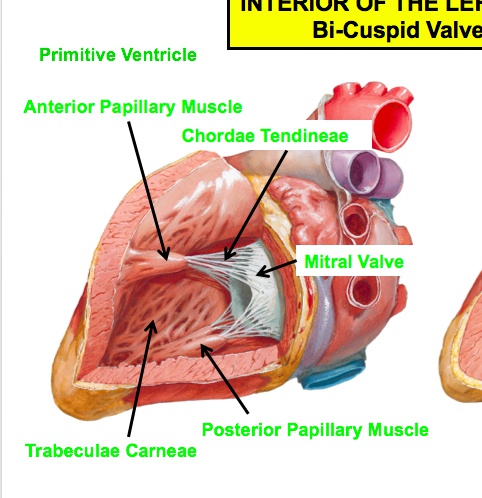
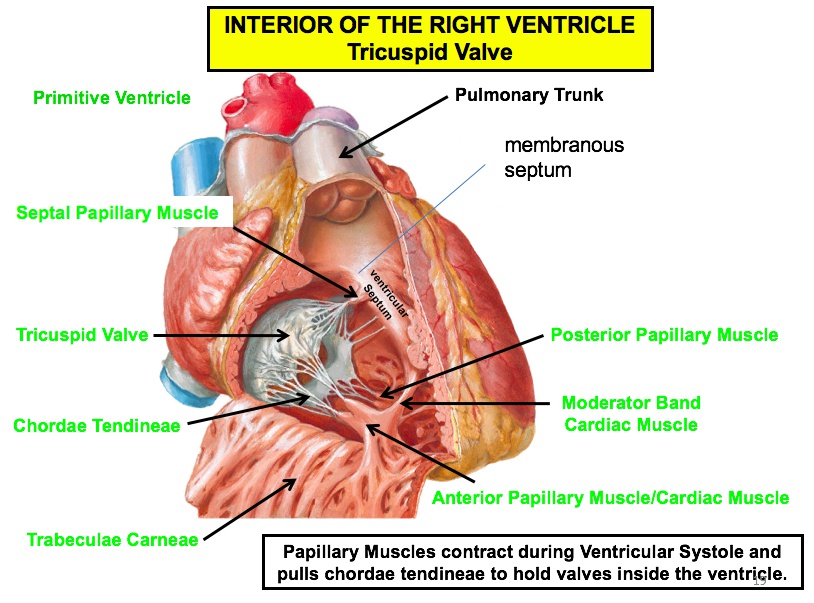
Trabeculate carneae
Thick bundles of muscle that give the right ventricle its rough texture; thicker than the pectinate muscles of the atria.
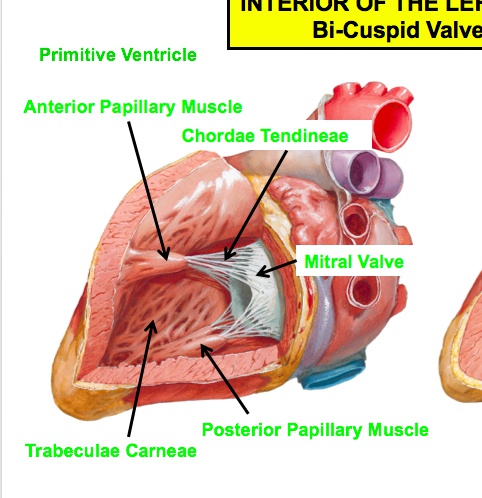
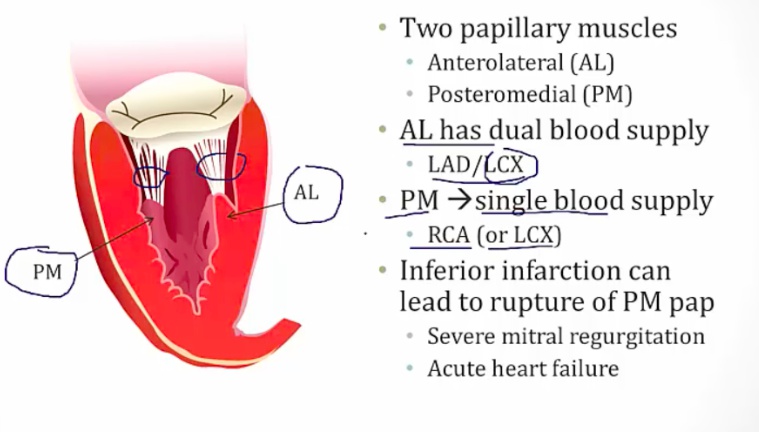
Papillary Muscles
Projections of ventricular muscle that are attached to the cusps of atrioventricular valves via the chordae tendineae preventing valvular prolapse during systole. Note: Please see associated image for the relationship of the three structures.
Septomarginal trabeculae
Aka moderator band.
Connecting bridge between the interventricular septum and the root of the anterior papillary muscle.
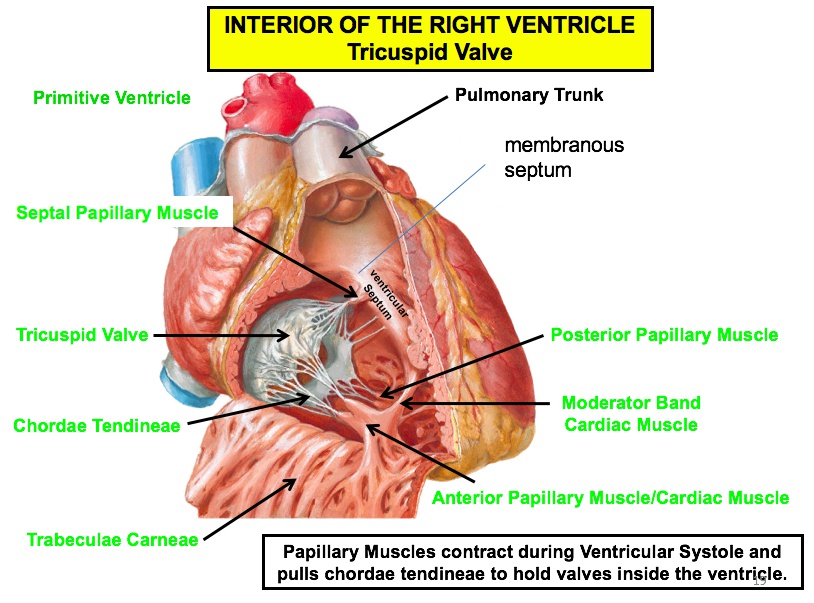
Chordae Tendinae
Fibrous cords that attach the papillary muscles to the valve cusps; the tension created by contracting papillary muscles and taut chordae tendinae prevent the cusps of the AV valve from prolapsing into the atrium as the ventricle contracts and the pressure on the valve increases.
Left Atrium
The most posterior chamber of the heart. Anterior to the esophagus. Thus, enlargement can cause:
- Dysphagia by compressing the esophagus
- Hoarseness by compressing the left recurrent laryngeal nerve.
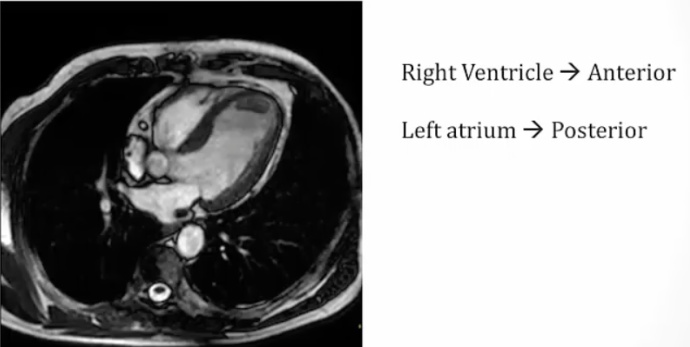
Esophagus: black hole between aorta and left atrium
Left Ventricle
The wall of the left ventricle is approximately 3x as thick as that of the right ventricle under non-pathological conditions.
Aortic Vestibule
Aka outflow tract of left ventricle.
The smooth portion of the left ventricle immediately proximal to the aortic valve.
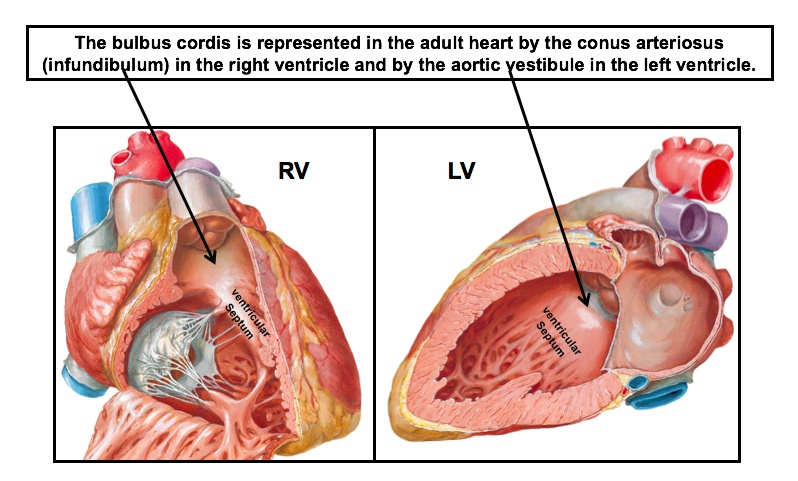
Valves
The anterior cusp of the mitral valve separates the outflow tract from the inflow tract (trabeculated tract).
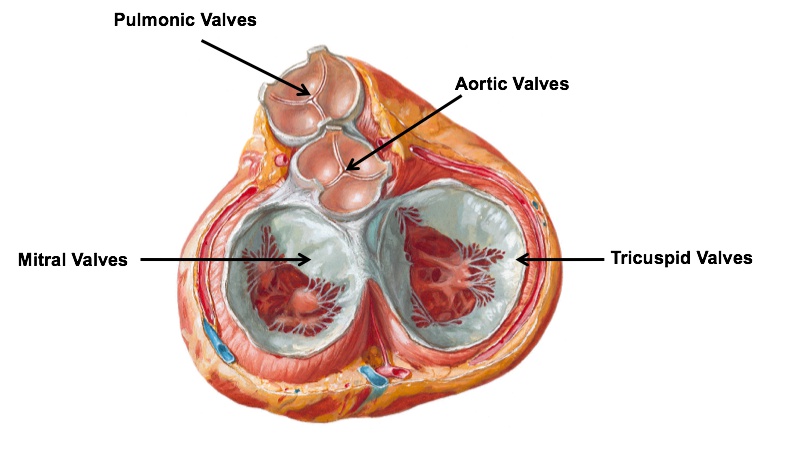
Aortic orifice
Includes the aortic valve and lies posteriorly and to the right of the pulmonary orifice.
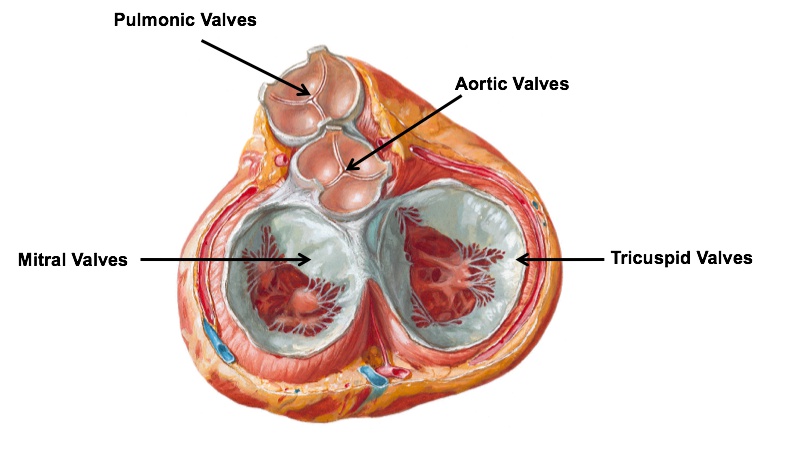
Left atrioventricular orifice
Defined by the bicuspid (mitral) valve; located posteriorly and to the left of the aortic orifice and to the left of the right atrioventricular orifice.
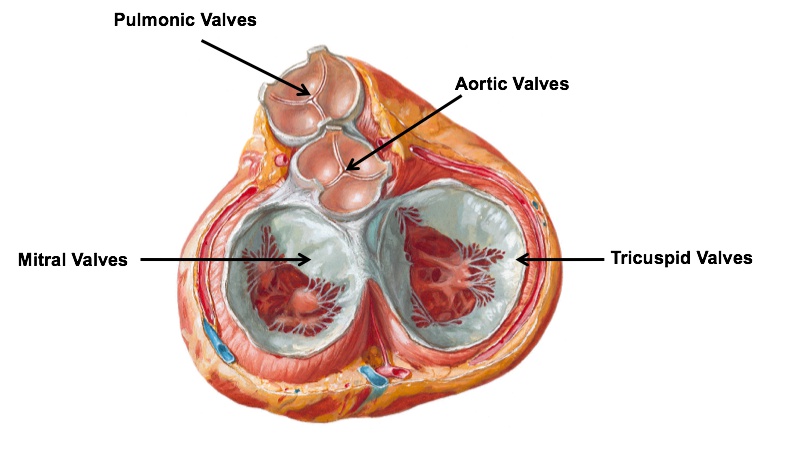
Mitral and Tricuspid Valves
Left atrioventricular (bicuspid/mitral) valve: The mitral valve is composed of anterior and posterior cusps; the anterior and posterior papillary muscles attach to the cusps via chordae tendinae
Right atrioventricular (tricuspid) valve: The right atrioventricular valve is formed by the anterior, posterior, and septal cusps.
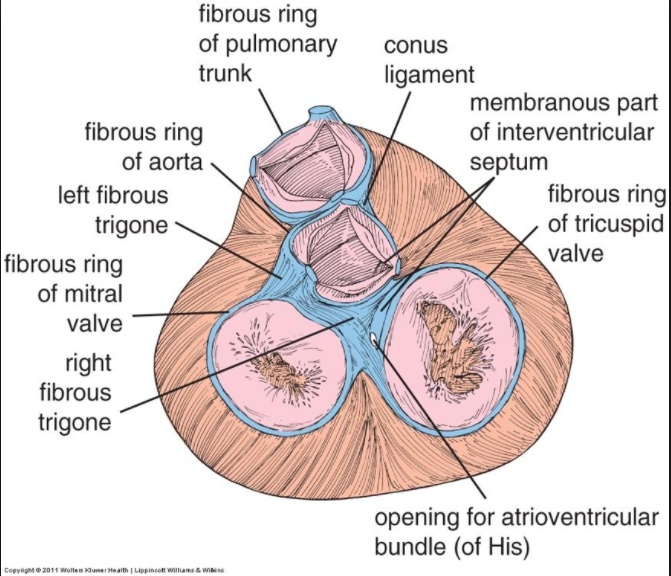
Anuli fibrosis
Fibrous rings of connective tissue that encompass each of the 4 valvular orifices; provide stable attachment sites and support for the cusps of the valves.
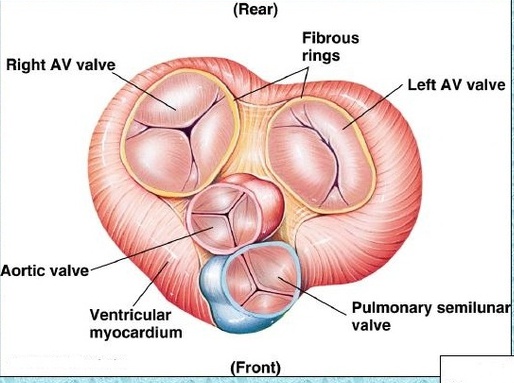
Fibrous trigones
Triangular-shaped fibrous connective tissue structures. The left side is between the annuli fibrosis of the aortic and mitral orifices; the right side is situated between the annuli fibrosis of the tricuspid, mitral, and aortic orifices. Function: Provide structural support for the valves of the heart and are components of the fibrous skeleton of the heart.
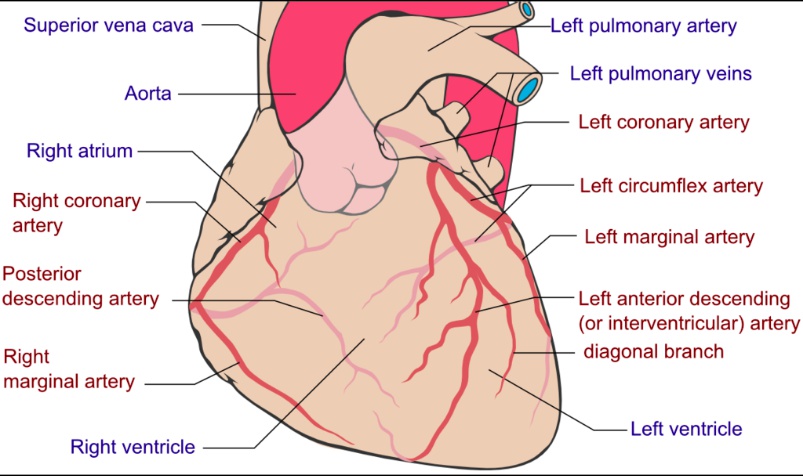
Cardiac Blood Supply
There are two main coronary arteries, the left coronary artery (LCA) and right coronary artery (RCA).
LCA
Originates from the left aortic sinus and bifurcates into:
- LAD (left anterior descending) artery, which gives off superficial (diagonal) and multiple deep (septal perforator) branches. anterior LV
- LCX (left circumflex) artery .
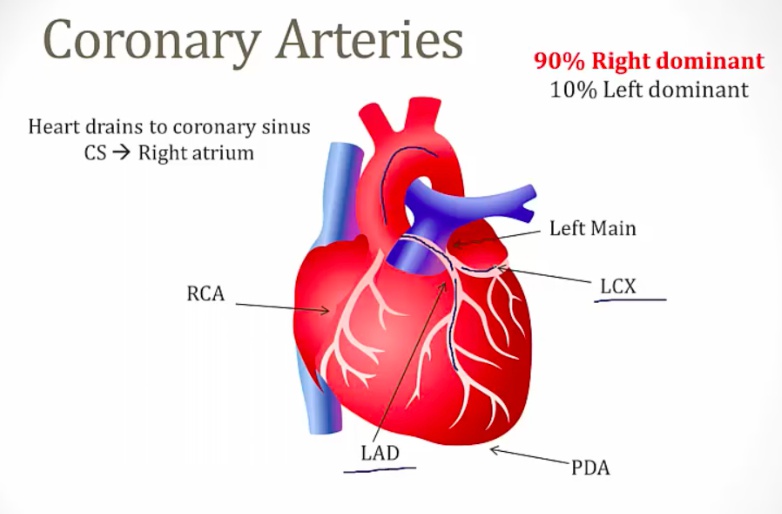
Supplied by the ascending aorta.
LCX
Wraps around the left border of the heart within the coronary sulcus.
Supplies:
- Posterolateral wall of left ventricle
- Anterolateral papillary muscle along with LAD.
LAD
Aka anterior interventricular artery.
Passes within the anterior interventricular sulcus toward the apex.
Supplies:
- Anterior wall of left ventricle
- Anterior 2/3 of the interventricular septum, or superior septum
- Anterolateral papillary muscle along with LCX.
Since the anterolateral papillary muscle is supplied by both the LAD and LCX, it is relatively resistant to infarction. In contrast, the posteromedial papillary muscle is more susceptible to ischemic injury since it is supplied by a single arterial branch: the PDA depending on dominance of the heart.
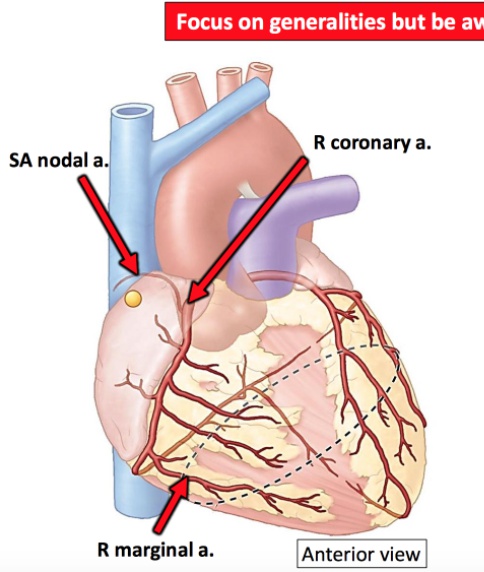
RCA
Originates from right aortic sinus and upplies:
- Right atrium and ventricle (inferior walls) via right marginal artery
- Left ventricle (diaphragmatic surface) via right marginal artery
- Posterior 1/3 of the interventricular septum or the inferior septum via PDA
- Right posteromedial papillary muscle via PDA
- AV node (in right-dominant individuals) via AV nodal artery from PDA
- SA node via SA nodal artery.
The RCA travels in the coronary sulcus between RA and RV and passes around right border of heart between the posterior and diaphragmatic surfaces.
Gives rise to the 4 branches below:
- Right marginal branch
- SA nodal artery
- PDA that also gives rises to AV nodal artery.
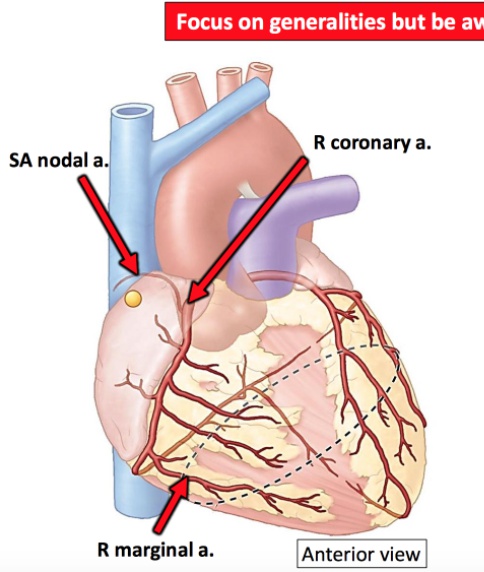
Right marginal branch
Arises from the RCA before it crosses the right border of the heart and travels along the acute margin just superior to the inferior border (see image); supplies the right ventricle.
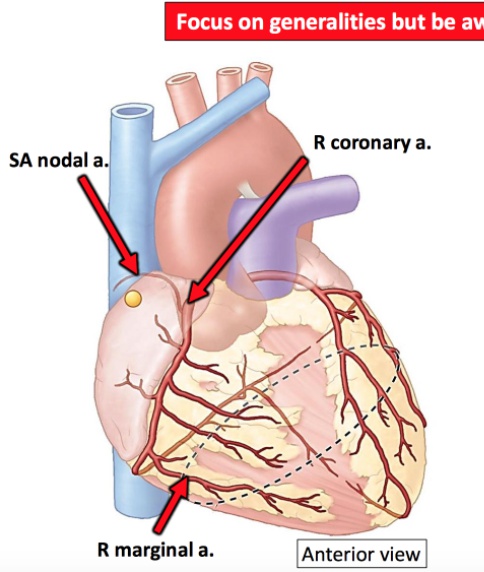
SA nodal artery
Has a variable course of travel and can encircle the SVC either posteriorly or anteriorly; during posterior circling, the artery travels left of the SVC, circles around the posterior aspect of the vessel, and emerges anteriorly on the right side of the SVC to supply the SA node.
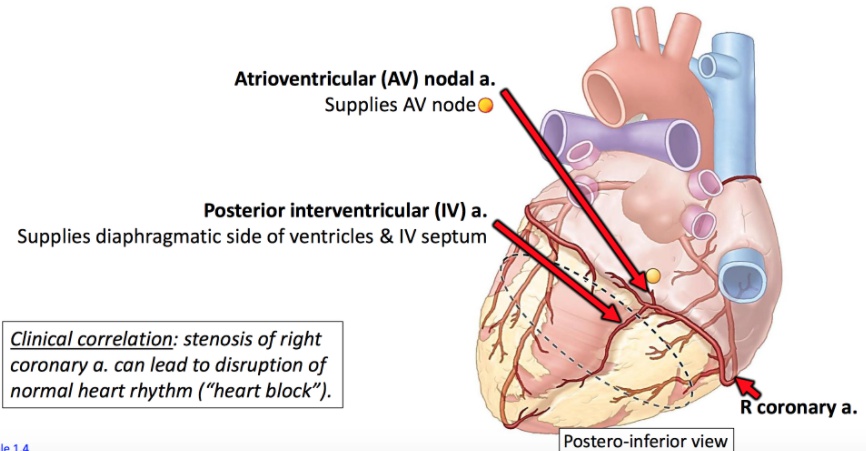
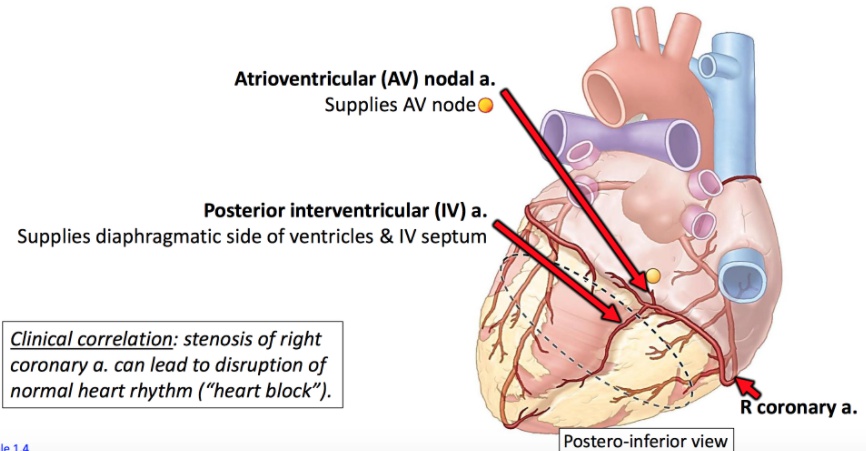
AV nodal artery
Supplies the AV node (90% of patients AV nodal artery, 10% LCX). Comes off off PDA.
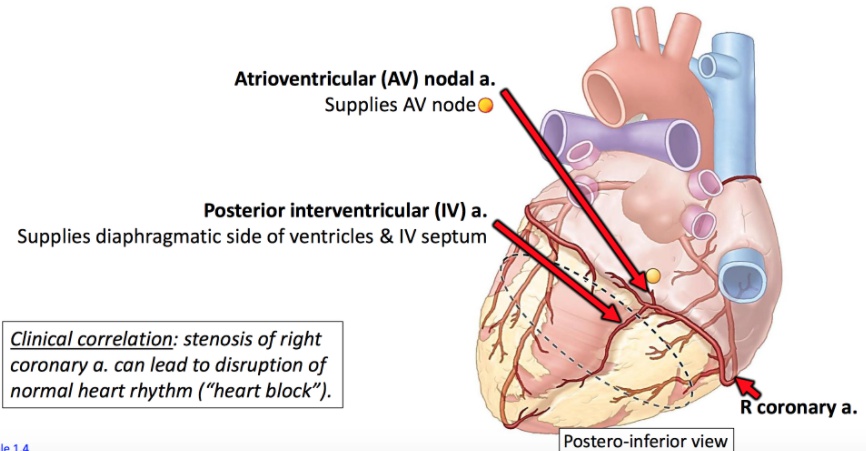
PDA
Aka posterior interventricular artery (PIV).
Emerges from the RCA after leaving the coronary sulcus and descends toward the apex of the heart (70% of population).
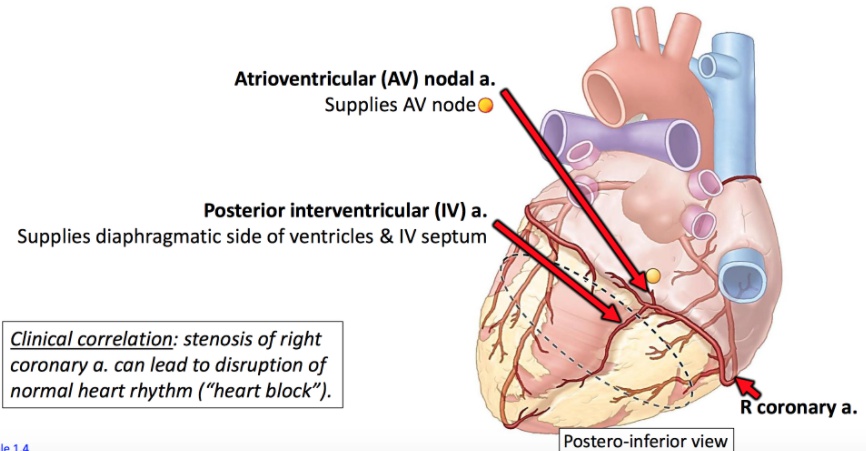
Supplies:
- Posterior 1/3 of interventricular septum or inferior septum
- Posterior walls of ventricles
- Posteromedial papillary muscle.
The artery that supplies the PDA is the structure that determines coronary dominance:
- Right dominant — PDA is supplied by the RCA (85% of population)
- Left dominant — PDA is supplied by the LCX (8% of population)
- Co-dominant — PDA is supplied by both the RCA and LCX (7% of population).
Heart Veins
Primarily drain to the coronary sinus, which empties directly into the right atrium.
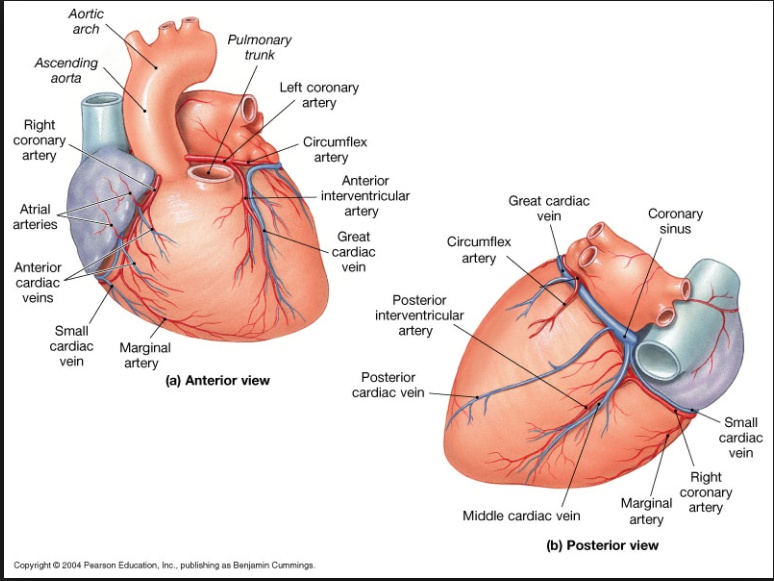
Great cardiac vein
Originates in the anterior interventricular sulcus; travels first with the left anterior descending artery (LAD) and then alongside the left circumflex artery (LCX).
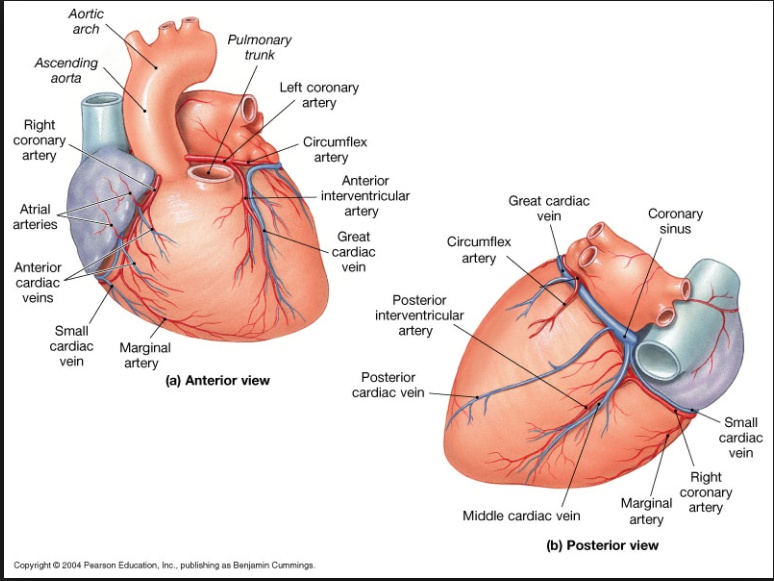
Middle cardiac vein
Ascends in the posterior interventricular sulcus with the posterior interventricular artery.
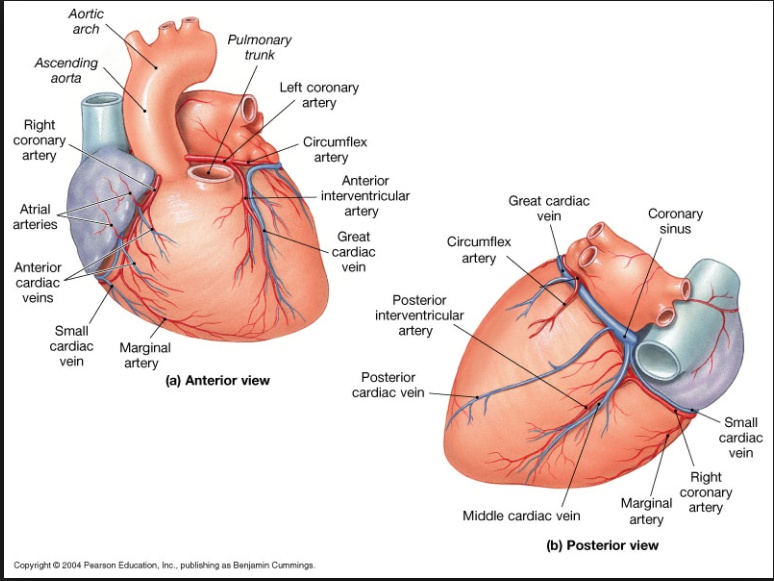
Small cardiac vein
Runs alongside the right marginal artery before traveling posteriorly in the right coronary sulcus with the right coronary artery; drains into the coronary sinus near its junction with the right atrium.
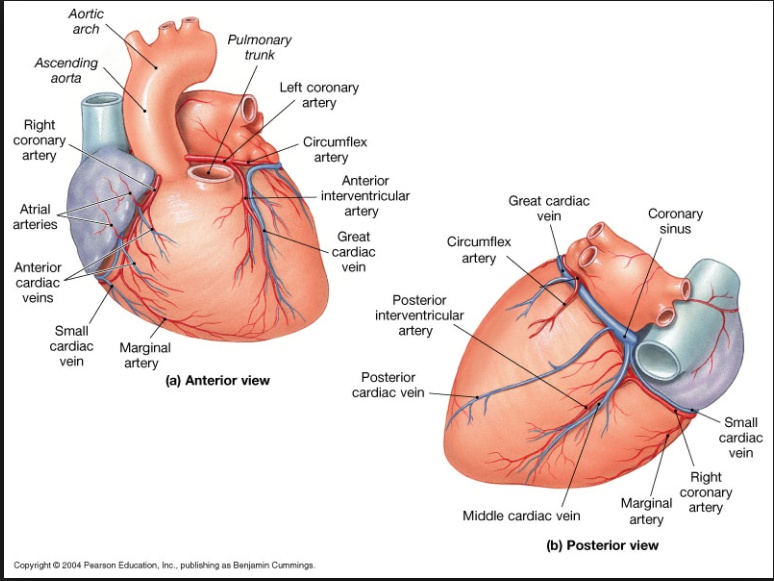
Anterior cardiac veins
Originate on the anterior wall of the right ventricle, cross the coronary sulcus, and drain into the right atrium.
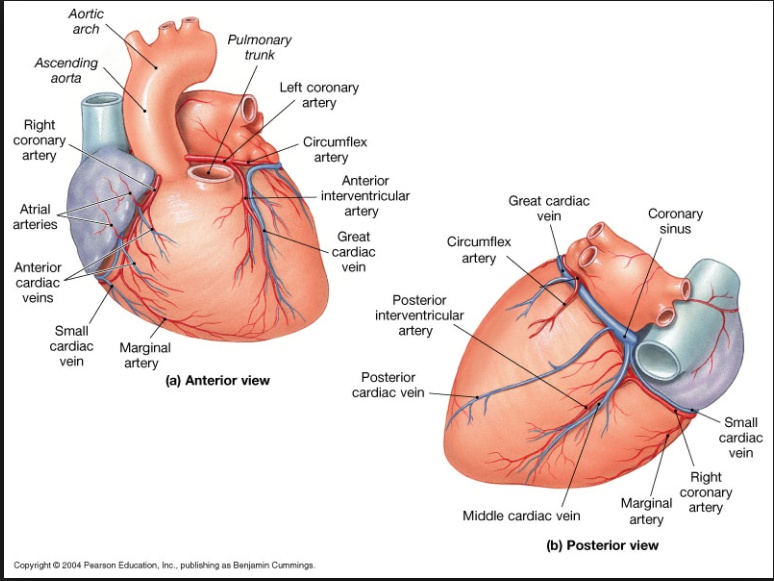
Smallest (thebesian) veins
Are found in the walls of myocardium of the 4 chambers of the heart; drain directly into the chambers.
aka venae cordis minimae.
Branches of aorta, ABC’S:
- Aorta
- Brachiocephalic trunk — Gives rise to the right common carotid and right subclavian
- Common carotid (left)
- Subclavian artery (left).
Brachiocephalic Artery
The first branch of the aortic arch, which immediately branches into the right common carotid and right subclavian arteries to supply the right arm, neck and head.
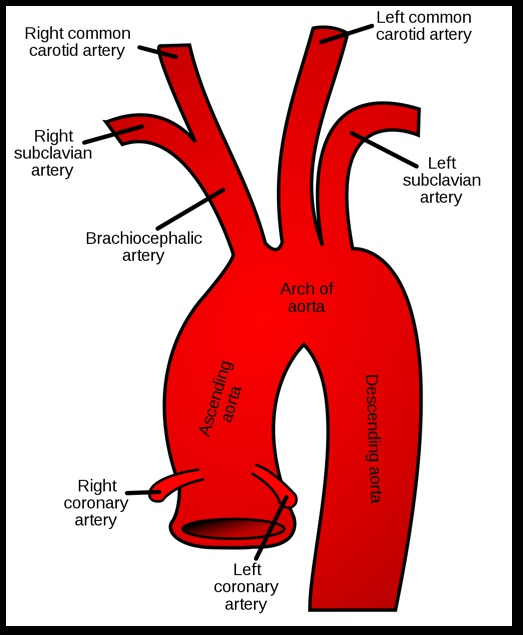
Left common carotid artery
The second branch of aortic arch, which supplies the left side of the neck and head.
Left subclavian artery
The third branch of aortich arch, which primarily supplies the left arm.
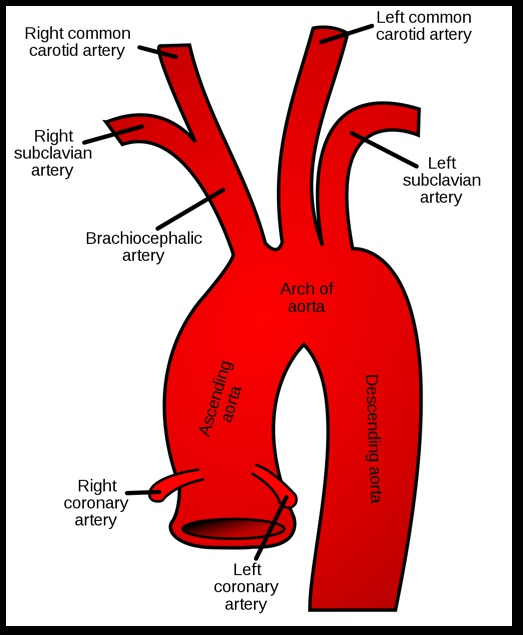
Both the right and left subclavian arteries give off multiple branches that enter and supply the neck region.
Pulmonary arteries
Branches of the pulmonary trunk and carry deoxygenated blood to the lungs.
Right pulmonary artery
Longer than the left and enters the hilum of the right lung between the right pulmonary vein and intermediate bronchus.
Left pulmonary artery
Shorter, enters the hilum of the left lung posterior to the left pulmonary vein and superior to the left primary bronchus.
Ligamentum arteriosum
A fibrous remnant of the ductus arteriosus attaching the left pulmonary artery to the aortic arch.
The relationship of the pulmonary artery to the bronchus can be remembered with the mnemonic: RALS.
- Right — Anterior (right pulmonary artery is anterior to right intermediate bronchus)
- Left — Superior (left pulmonary artery is superior to the left principal bronchus).
The internal thoracic (mammary) artery
Aka mammary artery.
The first caudal branch of the subclavian artery and runs inferiorly along the internal surface of the anterior thoracic wall.
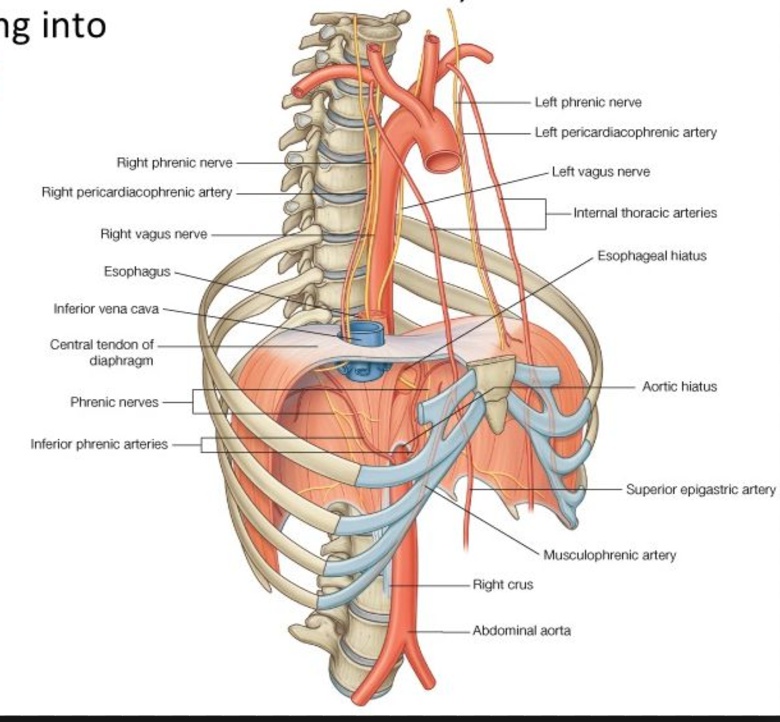
At the level of the 6th intercostal space branches into the musculophrenic and superior epigastric arteries.
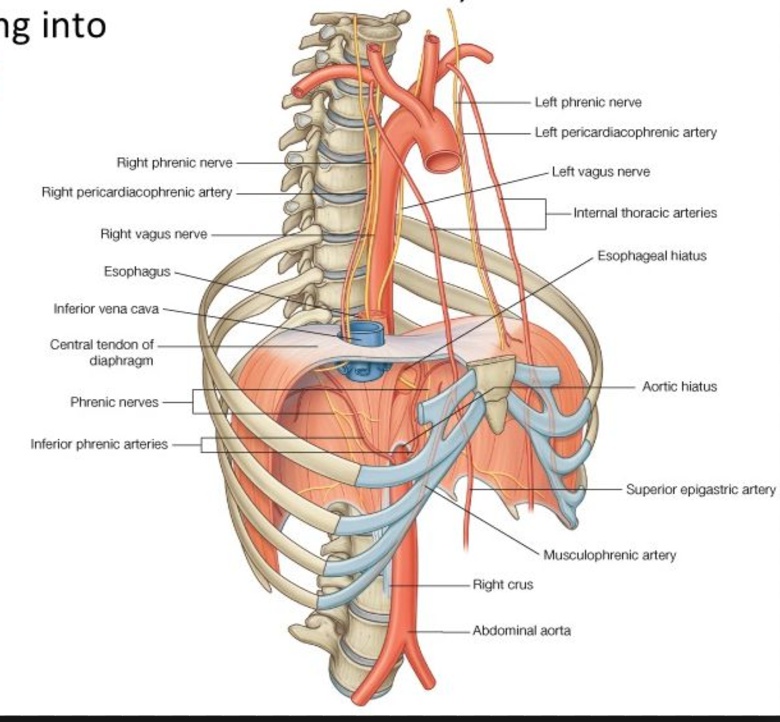
The thoracic aorta courses inferiorly along the thoracic vertebral bodies.
At the level of T12, thoracic aorta penetrates the diaphragm via the aortic hiatus and becomes the abdominal aorta.
Anatomical relationships for the diaphragm can be remembered with the mnemonic "I ate (eight/8) 10 Eggs Aat 12":
- IVC perforates diaphragm at T8
- Esophagus and vagus perforates diaphragm at T10
- Aorta, azygous vein, and thoracic duct, perforates diaphragm at T12.
The descending thoracic aorta gives off the following branches:
- Pericardial branches
- Bronchial branches
- Esophageal branches
- Mediastinal branches
- Posterior intercostal arteries
- Superior phrenic arteries
- Subcostal artery.